Podoconiosis is a non-filarial, non-infectious disease, caused by long-term exposure to red clay soil derived from volcanic rock which causes destruction of the lymphatic circulatory system in the feet and legs. Once lymphedema (Organic Lymphatic Vessel Disease) is established, the well-known cutaneous manifestations and natural progression of the disease are clear.
The infection is stated to occur mostly in childhood and the disease first becomes symptomatic in the early teens and affects both sexes. It starts first from the feet and then spreads up the legs to the level of the knees, and is caused by blockage of regional lymph nodes and vessels. Although both legs are involved, leg swelling tends to be asymmetrical.
Podoconiosis disease is most prevalent in resource-limited countries and especially among agrarian people who work barefoot, particularly in the neighborhood of volcanoes.
Podoconiosis symptoms include leg and foot pain, flare with exertion, itching, burning, swelling in the sole of the foot, marked soft tissue thickening, underlying bone changes, and bacterial infection. If left untreated or undertreated, the condition progresses toward Stage III Lymphedema, also called elephantiasis, characterized by large edema, and leathery pigmented feet. and lower leg disability and disfigurement. Read more about the signs, symptoms, and complications of lymphoedema HERE.
Lymphedema includes both Primary Lymphedema (a genetic condition) and Secondary Lymphedema (caused by various factors like surgery, radiation, infection, barefoot exposure to irritant soils, insects, etc). Podoconiosis is thus a Secondary Lymphedema, and its most advanced stage is known as "Elephantiasis". The elephantiasis stage (advanced lymphedema) is not something that is only related to podoconiosis/filariasis, or localized in poor and developing counties, but is also related to all the other causes of lymphedema, and can also be found in European and high-tech nations. Read about the myths and facts of elephantiasis HERE.
Lymphedema (Organic Lymphatic Vascular Disease) is due to impaired lymphatic drainage resulting in skin disease, characterized by persistent and progressive swelling, and abnormal thickening of the skin and subcutaneous connective tissue. Lymphedema is not just a localized swelling problem, but a condition that can affect multiple body systems, structures and functions, leading to a range of physical, physiological and psychosocial symptoms and complications.
Lymphedema arises when there is a disruption of lymphatic flow (Organic Impairment), leading to the buildup of lymphatic fluid. It is clear that no patient or their lymphedema is the same and neither is its progress. Some patients with lymphedema have few symptoms, and can easily do different degrees of physical activity, while others feel the strain, experience increased swelling with minimum effort, or even suffer varying degrees of disability and severe complications.
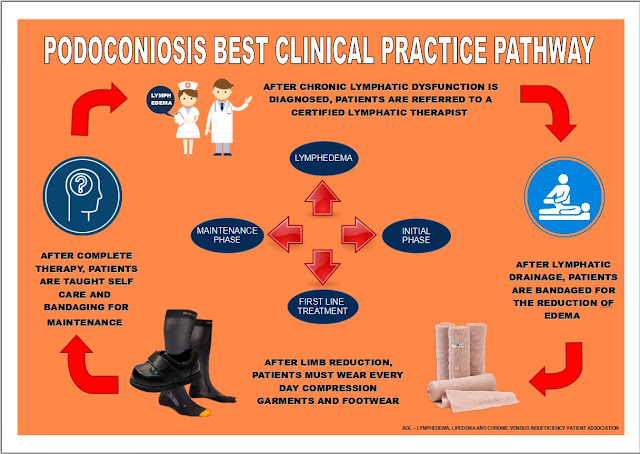
The good news for Podoconiosis is that established lymphatic dysfunction is treatable. Therapy of peripheral lymphedema is divided into conservative (non-operative) and operative methods. The best first-line non-surgical treatment for lymphedema, considered the "Gold Standard" treatment, is Complete Decongestive Therapy (CDT).
Complete Decongestive Therapy (CDT) is not limited to lymphedema stages I and II, and even late Stage III lymphedema (elephantiasis) improves greatly with good results in the majority of cases, thus preventing the need for debulking techniques.
Radical reductive ablative surgery (Charles Procedure), aimed to remove the diseased skin and subcutaneous tissue, should always be the last option, for it is frequently associated with significant blood loss, morbidity, infections, permanent disfigurement, and recurrence of symptoms.
The success of Complete Decongestive Therapy (CDT) depends on it being administered by an experienced certified therapist. CDT is considered safe, however, patients should consult with their physician before beginning treatment. Indications, contraindications, and the application of individual therapeutic measures depend on several factors: the stage of lymphedema at the start of treatment, comorbidities, the age of the patient, and the patient’s individual life circumstances.
Failure of CDT should be confirmed only when intensive non-operative treatment in a clinic specializing in the management of peripheral lymphedema and directed by an experienced clinical lymphologist has been unsuccessful.
In no way should this highly specialized treatment be replaced, due to the possible serious side effects, by edema reduction treatments carried out by non-specialists. Aggressive reduction of swelling can cause skin and vessel damage. Isolated compression therapy of the extremities without Manual Lymphatic Drainage (MLD), particularly in patients with lymphedema also affecting the quadrants of the trunk, may cause the shift of edema and increase swelling at the root of the extremity, and may even lead to genital lymphoedema.
Due to derangement of lymphatic function (Organic Lymphatic Vessel Disease) and resulting weak body defense, the limb with lymphedema is prone to repeated bacterial and fungal infections. Concerning Dermatolymphangioadenitis (DLA), also known as infectious cellulitis, studies have shown that swelling control is associated with a lower risk of cellulitis, and furthermore, that advanced degrees of chronic edema are a strong risk factor. Infectious Cellulitis can lead to sepsis (Septicaemia). Read more about lymphedema and Infectious Cellulitis HERE.
At the personal and work level, the majority of individuals affected by lymphedema cannot devote all hours of the day to exercise and limb elevation to retain the progression of edema, for they also need to attend to their daily chores and jobs, and this can only be achieved by wearing compression garments.
The daily use of standard bandages for lymphedema is not practical. Bandages lose pressure after application due to edema reduction, and they also tend to loosen and slip off when undertaking work that requires continuous physical activity, likewise, dirty bandages can also be an important source of infection. While bandages are mainly used for the initial phases of compression therapy, compression garments are recommended for the maintenance and long-term management of chronic conditions.
For the maintenance phase of lymphedema management, compression is the most important intervention. Compression garments are easy to use and achieve significant improvements in most patients without causing much discomfort. The beneficial value of applying compression stockings in the treatment of venous and lymphatic disease is supported by recommendations rated as Grade 1 evidence. Read more about what is the best treatment for elephantiasis HERE.
The use of footwear is very important for the prevention of Podoconiosis, but once chronic lymphatic dysfunction (lymphedema) is established, shoes alone are not enough to stop the advance of the disease. Scientific studies highlight the importance of compression therapy in controlling the progression of lymphedema.
Clinical results of interventions to control lymphoedema show that simple hygiene-based measures (skin care, exercises, elevation of affected limbs, standard bandages, and use of footwear) are necessary, but these alone are not enough to control the volume progression of the extremities. Read about what are the TRUTHS and MITHS about Elephantiasis and its treatment HERE.
Self-management strategies according to the chronic care model (CCM), where patients with chronic diseases should assume a leading role in their treatment to improve health status, daily functioning, and quality of life, should not be a substitute for the proper and necessary clinical treatment that this disease requires. Read about why the world is not treating a treatable disease like lymphedema HERE.
It has been scientifically demonstrated that the majority of individuals that suffer from Stage III Lymphedema, can´t be free of disability, disfigurement, and stigma that symptoms bring, and can´t be productive and live more fulfilling lives, without access to proper treatment. Strategies for morbidity management and disability prevention with simple intervention packages, that only focus on the care of acute infections and not on the necessary control of edema progression, will not halt the advance of lymphedema toward the final elephantiasis stage.
IMPORTANT NOTICE
Lymphedema is a serious chronic and progressive disease due to lymphatic dysfunction (Organic Lymphatic Vascular Disease). The clinical treatment of lymphedema is neither a cosmetic nor an aesthetic treatment. The treatment of lymphedema is to control its progression and alleviate the symptoms related to dysfunction of the lymphatic circulatory system.
To prevent and avoid serious complications associated with treatment, such as the possible displacement of edema to previously unaffected areas when compression therapy is applied for volume reduction, patients should use highly specialized and experienced therapists. Professional qualification and instruction delivered remotely online are not the same as live hands-on practical instruction in the clinical training and certification of lymphedema therapists, similar to all other rehabilitation, medical, and surgical training programs, and especially for developing the necessary manual skills to treat a disease as complex as lymphedema.
Patients should also take special care when choosing a Multidisciplinary Center of Reference for Lymphedema, as not all countries and centers provide the same treatment options. The best choice is a center of reference that provides Complete Decongestive Therapy (CDT), which is recognized as the Gold Standard treatment for lymphedema.
- Read more the best treatment option for Lymphedema HERE.
- Read about the principal functions of Manual Lymphatic Drainage HERE.
- Read about The differences between the two principal lymphedema treatment protocols HERE.
- Read about the strategies for the implementation of low-cost treatment options for Lymphedema HERE.
REFERENCES
(Click on the texts to read the research articles)
SCIENTIFIC SOCIETIES
PATHOPHYSIOLOGY
- lymphedema.
- Biology of Lymphedema
- Lymph vessels: the forgotten second circulation in health and disease
- Lymphatic Vessel Network Structure and Physiology
- Lymphatic System Flows
- Organ-specific lymphatic vasculature: From development to pathophysiology.
- The lymphatic vascular system: much more than just a sewer.
- The unresolved pathophysiology of lymphedema.
- Lymphedema: A Practical Approach and Clinical Update.
- Coagulation in Lymphatic System.
- Regulation of immune function by the lymphatic system in lymphedema.
- Oxidative stress in chronic lymphoedema.
- Regulatory T Cells Mediate Local Immunosuppression in Lymphedema.
- Hemostatic properties of the lymph: relationships with occlusion and thrombosis.
- Secondary lymphedema: Pathogenesis
- Gastrointestinal Lymphatics in Health and Disease
- Intestinal lymphangiectasia in adults
- Role of the lymphatic vasculature in cardiovascular medicine
- The lymphatic vasculature in disease
- Lymphoscintigraphic abnormalities in the contralateral lower limbs of patients with unilateral lymphedema.
- The Prevalence of Lower Limb and Genital Lymphedema after Prostate Cancer Treatment: A Systematic Review
- Peripheral Edema
- The lymphatic system and the skin. Classification, clinical aspects, and histology.
- Lymphedema and cutaneous diseases.
- Lymphedema and subclinical lymphostasis (microlymphedema) facilitate cutaneous infection, inflammatory dermatoses, and neoplasia: A locus minoris resistentiae.
- Serum Immune Proteins in Limb Lymphedema Reflecting Tissue Processes Caused by Lymph Stasis and Chronic Dermato-lymphangio-adenitis (Cellulitis).
- Lymphedema and subclinical lymphostasis (microlymphedema) facilitate cutaneous infection, inflammatory dermatoses, and neoplasia: A locus minoris resistentiae.
- Lymphatic Flow: A Potential Target in Sepsis.
- Infectious complications of lymphedema.
- Acute inflammatory exacerbations in lymphoedema.
- Inflammatory Manifestations of lymphedema.
- Cellulitis.
- Clinical features, microbiological epidemiology, and recommendations for the management of cellulitis in extremity lymphedema.
- Challenges of cellulitis in a lymphedematous extremity.
- Diagnosis and management of cellulitis.
- Cellulitis risk factors for patients with primary or secondary lymphedema.
- Oedema as a risk factor for multiple episodes of cellulitis/erysipelas of the lower leg.
- Prevention of dermatolymphangioadenitis by combined physiotherapy.
- Erysipelas: a common potentially dangerous infection.
- Malignant tumors as complications of lymphedema.
- Lymphedematous areas: Privileged sites for tumors, infections, and immune disorders.
- Lymphedema-related angiogenic tumors and other malignancies.
- Lymphedema: an immunologically vulnerable site for the development of neoplasms.
- Lymph stasis promotes tumor growth
- A retrospective analysis of Stewart-Treves syndrome in the context of chronic lymphedema.
- Stewart-Treves Syndrome
- Congenital lymphedema complicated by pain and psychological distress: case report
- Lymphatic Pain in Breast Cancer Survivors
- Does Manual Lymphatic Drainage Have Any Effect on Pain Threshold and Tolerance of Different Body Parts?
- Lymphedema therapy reduces the volume of edema and pain in patients with breast cancer
- Quality of life in patients with primary and secondary lymphedema in the community
TREATMENT
- Treatment of limbs lymphedema.
- Nonoperative treatment of lymphedema.
- Lymphedema: From diagnosis to treatment.
- Lymphedema-clinical picture and therapy.
- Physiotherapeutic rehabilitation of lymphedema: state-of-the-art.
- Diagnosis and management of lymphatic vascular disease
- Effective treatment of lymphedema of the extremities.
- Lymphoscintigraphic aspects of the effects of manual lymphatic drainage.
- Intensive Treatment of Lower-Limb Lymphedema and Variations in Volume.
- Effectiveness and safety of Complete Decongestive Therapy of Phase I.
- Therapeutic Efficacy of Complex Decongestive Therapy in the Treatment of Elephantiasis of the Lower Extremities.
- Effects of Phase I complex decongestive physiotherapy on physical functions and depression levels in breast cancer-related lymph edema.
- Does lymphoedema bandaging reduce the risk of toe ulceration?
- Study of 700 referrals to a Lymphedema Program.
- Worldwide assessment of healthcare personnel dealing with lymphoedema.
- Földi M, Földi E. Földi’s textbook of lymphology for physicians and Lymphoedema therapists.
- Fluid Shifts Induced by Physical Therapy in Lower Limb Lymphedema Patients
- Visualization of Accessory Lymphatic Pathways, before and after Manual Drainage, in Secondary Upper Limb Lymphedema Using Indocyanine Green Lymphography
- The risk of genital edema after external pump compression for lower limb lymphedema.
- The management of genital lymphoedema
- The management of deep vein thrombosis in lymphoedema: a review.
- Lymphedema-associated comorbidities and treatment gap.
- A study of the advantages of elastic stockings for leg lymphedema.
- Indications for medical compression stockings in venous and lymphatic disorders: An evidence-based consensus statement.
- Medical compression stockings for chronic venous diseases and lymphedema: Scientific evidence and results of a patient survey on quality of care.
- Impact of Compression Therapy on Cellulitis (ICTOC) in adults with chronic edema: a randomized controlled trial protocol.
- Compression Therapy Is Cost-Saving in the Prevention of Lower Limb Recurrent Cellulitis in Patients with Chronic Edema.
- Occupational leg edema-use of compression stockings.
DISABILITY
- Disability and lymphedema.
- Lymphedema and employability.
- Worse and worse off: the impact of lymphedema on work and career after breast cancer
- Functioning in lymphedema from the patient's perspective using the International Classification of Functioning, Disability and Health (ICF).
- Unilateral upper extremity lymphedema deteriorates the postural stability in breast cancer survivors
- Postural Stability in Patients with Lower Limb Lymphedema
- Disability, psychological distress and quality of life in breast cancer survivors with arm lymphedema
DISFIGUREMENT
- Adjusting to disfigurement: processes involved in dealing with being visibly different
- Quality of Life in Cancer Patients with Disfigurement due to Cancer and its Treatments
- Quality-of-life and body image impairments in patients with lymphedema
- Association of lower extremity lymphedema with pelvic floor functions, sleep quality, kinesiophobia, body image in patients with gynecological cancers
QUALITY OF LIFE
- The impact of lower limb chronic oedema on patients' quality of life
- Quality of life in patients with primary and secondary lymphedema in the community
- Evaluating the effect of upper-body morbidity on quality of life following breast cancer treatment.
- Functionality and quality of life of patients with unilateral lymphedema of a lower limb: a cross-sectional study
- The effect of complete decongestive therapy on the quality of life of patients with peripheral lymphedema
PSYCHOSOCIAL IMPACT
- Psychosocial Impact of Lymphedema.
- Associations between chronic disease, age and physical and mental health status
- A network analysis of psychological flexibility, coping, and stigma in dermatology patients
- 'Abandoned by medicine'? A qualitative study of women's experiences with lymphoedema secondary to cancer, and the implications for care
- People are neglected, not diseases.
- Chronic edema/lymphoedema: under-recognized and under‐treated.
- Lymphatic Medicine: Paradoxically and unnecessarily ignored.
- Medical education: a deficiency or a disgrace.
PEDIATRIC LYMPHEDEMA
- NORD: Rare Disease Database - Lymphedema
- Medical management of lymphedema.
- Primary lymphedema in childhood.
- An approach to familiar lymphedema
- Pediatric Children Lymphedema
- Primary Lymphedema French National Diagnosis and Care Protocol (PNDS).
- Lymphatic filariasis: an infection of childhood.
- Lymphatic filariasis in children: clinical features, infection burdens and future prospects for elimination.
- Podoconiosis: Clinical spectrum and microscopic presentations.
- Podoconiosis: A Possible Cause of Lymphedema in Micronesia.
- A cross-sectional study to evaluate depression and quality of life among patients with lymphoedema due to podoconiosis, lymphatic filariasis, and leprosy.
- The impact of acute adenolymphangitis in podoconiosis on caregivers.
- Neglected tropical diseases and disability-what is the link?
- Locomotor disability in bancroftian filarial lymphoedema patients.
- Neglected patients with a neglected disease?
- Neglected tropical diseases and mental health: a perspective on comorbidity.
- People are neglected, not diseases.
- Addressing Inequity: Neglected Tropical Diseases and Human Rights.
- Neglected Tropical Diseases, Conflict, and the Right To Health.
- Peripheral Edema
- Phlebolymphedema
- Understanding Chronic Venous Disease: A Critical Overview of Its Pathophysiology and Medical Management
- Role of the lymphatic vasculature in cardiovascular medicine
- Communication between lymphatic and venous systems
- Phlebopathies and occupation
- Phlebopathies and workers
- Evidence of health risks associated with prolonged standing at work and intervention effectiveness
- Leg edema formation and venous blood flow velocity during a simulated long-haul flight



.gif)


